Healthcare Innovation: Lessons from COVID-19

This blog is written by Richard Holti, Professor of Professional Learning and John Storey, Professor of Human Resource Management, both based in the OU Business School. They are the authors of Innovating Healthcare: The Role of Political, Managerial and Clinical Leadership (Routledge 2020).
It is widely anticipated that COVID-19 is likely to be a game-changing phenomenon. Health service provision and organisation, it is argued, are unlikely to remain as they were prior to its onset. Yet, the design and delivery of that new normal, if it is to be efficient and effective, will require imaginative and skilful innovation work by actors at many levels.
In order to evaluate the key lessons for appropriate innovation in healthcare, we first review key aspects of the experience of COVID-19 in England before moving on to summarise the findings from our research of the previous attempts to innovate healthcare which are most relevant under the new circumstances.
The COVID-19 experience so far
The COVID-19 experience has delivered a number of shocks to the system; indeed, the extent and severity of the perturbation has merited the frequent use of the term ‘crisis’. This, in turn, has prompted novel behaviours and a willingness to follow central directives. It has exposed strengths and weaknesses in the way health and social care, including public health, are organised and delivered. There is much talk of ‘learning lessons’ and there is laudable intent to shape the post-COVID service in new ways. But it cannot be assumed that these good intentions will be easily acted upon or easily delivered. A good place to start is to be alert to lessons from systematic studies of previous attempts to innovate healthcare. We spent nearly a decade researching service redesign attempts in the NHS and a summary of results was published in the book Innovating Healthcare: The Role of Political, Managerial and Clinical Leadership (Routledge 2020). Below, we seek to discuss some of the highlights as they relate to moving forward in the light of COVID-19 before drawing on that research to highlight a few key issues relevant to healthcare innovation.

In many respects, the NHS coped quite well with COVID-19: for example, it was agile enough to reconfigure, at speed, its hospital theatres and wards and related facilities so as to be able to focus on handling an influx of COVID-19 patients. The Nightingale hospitals were equipped, an parmy of partner organisations recruited, and as a result of all these efforts the hospitals were not overwhelmed. Likewise, the wholesale shift to telephone and online consultations in primary care and other community services has in many ways been a remarkable innovation which has surely accelerated a trend which was hitherto growing relatively slowly.
But, at the same time, the crisis has exposed significant shortcomings in both organisation and leadership. For example, the flaws in the structural divide between health and social care have been starkly revealed. The prioritisation afforded to COVID-19 in the hospitals was accompanied by a neglect of other health needs including cancer diagnosis and treatment. Patients and residents in nursing homes and care homes were neglected in the rush to focus on the emergency departments. This has impelled renewed and more emphatic calls to ‘integrate’ social care with the NHS. The size of that challenge is very large and remains so, albeit with a new level of awareness. Even within the boundaries of the NHS itself, there is organisational complexity which has been highlighted as the novel Coronavirus emerged and spread. Political control was made clear with the guidance and legislation along with the daily briefings from Downing Street. Managerial leadership in the shape of NHS England (NHSE) maintained a low profile. Primary Care and the Accountable Care Organisations (ACOs) were likewise in little evidence, conversely, the role of the acute hospitals (and Intensive Care in particular) was thrust firmly centre stage. The shortages of intensive care beds raised new questions about the predominant emphasis over previous years of policy formation in favour of cutting hospital beds, based on an assumption that public health was best served by a health service geared towards community-based services that might intervene early in the development of long term conditions such as heart disease and diabetes.
 Testing and tracing is one key area where the national infrastructure has clearly struggled. Testing outside of healthcare contexts was largely abandoned as infection rates accelerated in late March. However, as infection rates have fallen and exit from lockdown has become the central concern, testing, tracing, and infection control more broadly, are widely regarded as crucial, albeit still struggling. The division of responsibility between the Department of Health’s newly assembled testing capacity, Public Health England and its national system for contract tracing (including a hastily contracted private sector technical and administrative infrastructure), and the local authority-based Directors of Public Health and their established workforces, became an evident problem. The government has recently announced that responsibility for handling pandemics will be taken away from Public Health England and allocated to a new national institute. Meanwhile, serious doubts continue to be voiced about the adequacy of the testing and tracing system to support the emergence from lockdown.
Testing and tracing is one key area where the national infrastructure has clearly struggled. Testing outside of healthcare contexts was largely abandoned as infection rates accelerated in late March. However, as infection rates have fallen and exit from lockdown has become the central concern, testing, tracing, and infection control more broadly, are widely regarded as crucial, albeit still struggling. The division of responsibility between the Department of Health’s newly assembled testing capacity, Public Health England and its national system for contract tracing (including a hastily contracted private sector technical and administrative infrastructure), and the local authority-based Directors of Public Health and their established workforces, became an evident problem. The government has recently announced that responsibility for handling pandemics will be taken away from Public Health England and allocated to a new national institute. Meanwhile, serious doubts continue to be voiced about the adequacy of the testing and tracing system to support the emergence from lockdown.
The persistent dilemma of central versus devolved responsibility has been highlighted in several other ways. The decisive and rapid installation of the Nightingale Hospitals was indicative of the potential efficacy of decisive centre-led action. But, the confusion over the appropriate sourcing and distribution of personal protective equipment (PPE), testing equipment, testing facilities, and ventilators underlined the problems associated with lack of clarity concerning responsibility for supply.
Related to the centre-versus-local issue was the role of the private sector in providing equipment and consumables. The centre seemed to favour large suppliers and much publicity was given to the potential role of Dyson and other big companies; meanwhile, large numbers of small, local, suppliers were reportedly neglected and even ignored.
Summarizing so far, the COVID-19 experience has underlined the need for some critical changes and has placed a premium on skills for innovation. Some innovations have been achieved with remarkable speed, whilst others that are equally crucial have proved much more problematic. Hence, we turn next to a review of the lessons from numerous past attempts to innovate in the NHS with a view to assessing which of these might be most pertinent in the new COVID-19 and post-COVID world.
Lessons from previous innovation attempts
We found that the many previous attempts to innovate in the NHS operated both on a large national scale and on a small local scale. The linkages between these were often found to be crucially important. Many of the attempted top-down reforms and innovations failed to gain traction until picked up and re-worked at local level by agents who re-imagined the service offer and were thus able to operationalise them in practice.
System reform attempts rarely start with a blank canvass. There are established routines, protocols and commitments which guide behaviour. People, and the services they routinely deliver, are embedded in institutions. Considerable effort is expended in maintaining these institutions. Indeed, a significant number of leaders, at all levels, will already be engaged in some existing change initiative which they are seeking to progress and in which they may already be heavily invested. It is possible that a COVID-inspired initiative and/or priority may be enlisted to justify and add momentum to such existing forms of institutional work. Where, conversely, new priorities and imperatives challenge existing initiatives, time and effort may need to be spent in backing away from the ongoing work.
Our analysis of previous attempts to innovate in healthcare highlighted certain common patterns in those cases where some success had been achieved. We found that the ‘institutional work’ of breaking with previously established patterns of service delivery and establishing new ones typically occurred in three sub-phases: instigating work, implementing work and embedding work. During each of these, those engaged in making something new happen had to manage three inter-connected aspects of building a new way of delivering health care. Innovations, we found, were only sustained through a process containing the threefold processes of initiate, build, and embed:
-
A new network of professionals: bring together a new grouping of disciplines, occupations or specialisms needed to do something new or do an existing thing in a new way
-
A compelling moral justification and shared ethos: articulate a rationale for the innovation and build commitment to it amongst those involved, on the basis that it is the best use of professional expertise and other resources, for delivering results to service users and society
-
An effective operating model: a set of practices and related scientifically grounded concepts that allow professionals to deliver the innovative service smoothly, effectively and to a verifiable standard.
What is distinctive about COVID-19, in contrast to many of the examples of change in health systems which we studied, is that the acute level of ‘crisis’ awareness means that COVID-impelled directives and guidance are accorded an urgency and sense of priority beyond more ‘normal’ messages. Surmounting the prospect of collapsing services provides a pressing and clear moral justification, impelling professionals to accept more readily that there is a compelling need to work in new configurations according to much more stringent concepts and practices of infection control than most have previously encountered. So, the ‘instigating’ phase is much compressed – ways of working change more readily because of the widespread recognition of urgency in a crisis. Such times may be used to re-set priorities in a manner which can provoke speedy disruption to established practices and taken-for-granted assumptions.
Yet even this may not be enough. A recent account in the BMJ reported the experience of a doctor who was recruited as a contact tracer for the Public Health England tracing service. However, she reports how roles were unclear and interfaces between systems cumbersome, and a shared ethos binding the disparate parties and systems together was sadly lacking. Much of the required work of instigating and implementing this new ensemble of practices was evidently remaining to be achieved.
Even in those cases where innovations have made it through instigation to effective implementation, a subsequent key issue is whether they will become embedded. It seems likely that a deciding factor will be whether what happened during the crisis can continue to drive and establish a radically revised set of priorities, relationships and ways of working, versus a drift back to a resumption of behaviours and routines practised prior to the disruption. Our research on previous innovations suggests that much will depend on the strength and vitality of the informal networks that carry the sense of what a new way of working involves and why it is important. These networks often bring together people from different professions or occupations and can be significant sites for the crafting of new justifications for what it is right and proper to deliver, as well as the detailed techniques for doing so. If these networks find ways of connecting themselves with wider streams of thinking about what is of value in society, they are more likely to continue to win resources and to persist. So, the future of the test and trace system is likely to depend on an expanding interdisciplinary network of professionals who can make the complex interfaces between agencies work and at the same time act as advocates for the value to be gained from continued investment. But it will also depend on recognition amongst the general public and within political hierarchies that future pandemics, and indeed a resurgence of the current one, are possible and need to be planned for.
Finally, the acute awareness of critical issues such as the under-investment in key parts of the system, the shortcomings in supply chain management, the neglect of social care and of nursing and care homes along with other emergent failings, could potentially be used to impel corrective action. Here, innovators with a foot in different professional worlds can play a key role. Conversely, we know from past experience that there will be matching tendencies for the multiple and diverse parts of the system to seek to revert as soon as possible to former, familiar ways. A key question then, is how far different professional groups choose to identify with their established roles and organisational remits, or see their future value and resource-worthiness in terms of some of the new possibilities that the crisis has brought into view.
Photo credits:
Healthcare workers getting ready for work
18/03/2020. Photo taken by Francisco Àvia_Hospital Clínic.
Nightingale Hospital London for COVID-19
27/03/2020. Nightingale Hospital London for COVID-19. Picture by Andrew Parsons / No 10 Downing Street.
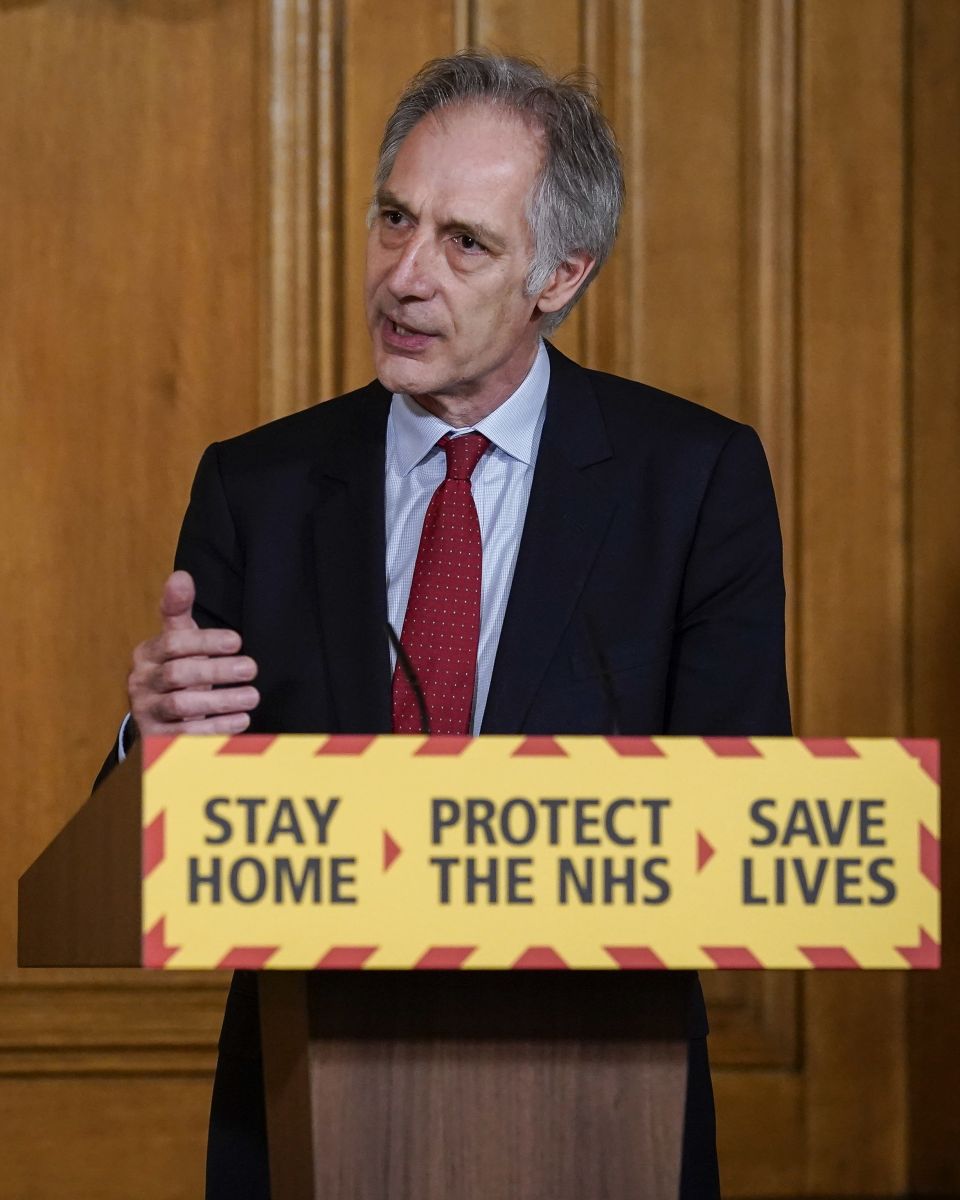
Coordinator of the National Testing Effort, Professor John Newton at the COVID-19 Presser 28/04
28/04/2020. Coordinator of the National Testing Effort, Professor John Newton at the daily digital press conference in No10 Downing Street on COVID-19. Picture by Andrew Parsons / No 10 Downing Street

Upcoming Events
Doing Academia Differently: Professional Development Symposium for Doctoral Students and Early-Career Academics
Tuesday, March 10, 2026 - 09:00 to 17:00
Michael Young Building, The Open University, Walton Hall, Milton Keynes, MK7 6BB
This one-day symposium on ‘Doing Academia Differently’ will provide inspiration and support for PhD and early-career academics to approach the complex tensions and dilemmas of contemporary academia in new and creative ways.
International Women’s Day: Supporting diverse new motherhoods for work inclusion
Thursday, March 12, 2026 - 11:30 to 12:30
Online Webinar - link below
Motherhood can have a particularly negative impact on employment for ethnic minority women. They are more likely to leave employment after the birth of their first child or to suffer workplace discrimination as a result. Wenjin Dai and Francesca Calo of The Open University Business School,...